Care Package
By Susan Spencer
Telegram & Gazette Staff
The woman, an adult with intellectual and developmental disabilities as well as significant mental health issues, was repeatedly in and out of the hospital emergency department.
Hospital personnel weren’t sure what more they could do once her immediate health crisis was stabilized.
The woman’s medical bills, covered by MassHealth, the state’s Medicaid program, were mounting with her frequent trips to the ER.
Once her therapist was brought into the loop, hospital staff would learn that the woman struggled with isolation and was using the ER not just for her medical crisis but also to alleviate loneliness.
She also needed stable housing but was overwhelmed with keeping on top of her bills.
In the traditional health care system, the multiple components needed to help this woman aren’t easily connected. Medical services would be arranged and paid for by one system. Socialization programs and housing support wouldn’t be part of that picture.
“One of the jobs of the care coordinator is to know all of the services that are out there and make sure these MassHealth recipients are hooked up with everything they need. This ties it all together.”
Michael Seibold, Director of Community Services at Alternatives

Robert Paquette smiles and takes program supervisor Joe Gulcius’s hand Feb. 15 at Alternatives in Whitinsville.
[PHOTOS/EDD COTE]
Under a new health reform model about to launch March 1, which will make accountable care organizations and managed care organizations financially responsible for the quality, total cost and care experience for more than 850,000 MassHealth members statewide, medical providers will have new flexibility to work with other types of agencies to care for people with complex needs.
Starting June 1, agencies known as community partners for behavioral health or long-term services and supports will work with ACOs to coordinate a wide range of services, in part to keep them from cycling in and out of the ER.
MassHealth has contracted with 27 community partners across the state.
The program is part of a five-year federal Medicaid waiver, which state officials said provides $1.8 billion in new federal spending to support the transition, including spending for care coordinators and electronic record systems.
Worcester-based Seven Hills Foundation is the lead agency for the Massachusetts Care Coordination Network, or MCCN, one of the community partners that puts in place long-term services and support for people with disabilities and other complex medical needs.
Other members of MCCN include Advocates, Brockton Area Multi-Services Inc., HMEA, Boston Center for Independent Living and BayPath Elder Services. MCCN provides services in Central, Northeast and Southeast Massachusetts.
Kathleen M. Jordan, executive vice president and CEO of Seven Hills Foundation, said that under the new care coordination model, as soon as it is known that the woman who makes frequent ER visits is at the hospital, MCCN can connect her with a day program to address her isolation and work with the housing authority to help her find a permanent home.
Once the “pieces of her puzzle are coming into place,” Ms. Jordan said, she takes her medications more consistently and her health is stabilized.
“We see instance after instance where looking at the whole person has a dramatic effect on medical utilization,” Ms. Jordan said.
Ms. Jordan and Christine Lens, director of MCCN, said that managed care organizations didn’t traditionally know how to manage populations with intellectual and developmental disabilities or chronic behavioral health needs.
The new MassHealth model forces ACOs and MCOs to work with community partners such as MCCN to understand these populations and to find more efficient and effective care.
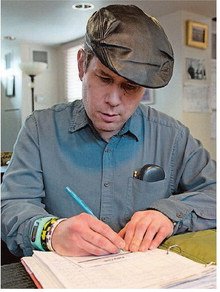
Matt Albee Jr. keeps track of his finances Feb. 15 in his Whitin Mill apartment in Whitinsville.
“A lot of people that have chronic illness have underlying depression,” Ms. Lens said. “To meet the emotional need with that is critical to turning it around.”
People with complex health care needs also account for a disproportionate share of MassHealth spending, and one of the goals of the program is to rein in total costs of care.
Health reform is trying to move to “value-based purchasing,” providing integrated service and support, according to Kenneth J. Bates, president and CEO of The Bridge of Central Massachusetts.
The Bridge is one of five organizations in another community partner group that works with ACOs in Central Massachusetts, called Central Community Health Partnership.
Other members of CCHP include Alternatives, AdCare, LUK Inc. and Venture Community Services. CCHP community partners offer both behavioral health and long-term services and supports.
Mr. Bates said the push to restructure health care delivery came from “the lack of integrated care, specifically behavioral health and medical care,” in the traditional model. “Payers of care are realizing integrating care has real benefits,” he said.
Michael Seibold, director of community services at Alternatives, based in Whitinsville, said the goals of care coordination were to enhance communication and collaboration between individual service providers and support programs, ensure that the individual uses the services they need in the most economical way, and improve the individual’s overall satisfaction as a result of better coordination among service providers.
The interdisciplinary team of nurses, clinicians, care managers, recovery coaches and care coordinators can serve people living in all settings, whether in a medical or long-term care facility, a group home, their family home or elsewhere.
Mr. Seibold highlighted several services offered by Alternatives that complement medical care provided to adults with psychiatric or developmental disabilities.
In one of three apartments in the renovated Whitin Mill at Alternatives’ main office in Whitinsville, two men, Matthew Albee Jr. and Robert Paquette, share an apartment and work with Alternatives staff on individual service plans, personal goals and skill development.
Program Manager Ronald Balkcom and Program Supervisor Joseph Gulcius talked with Mr. Albee about his health goals last week.
“Eating healthy, drinking healthy, exercise” were three goals Mr. Albee reported. He said he ate healthy snacks including fruit and celery, and goes for walks at River Bend Farm in Uxbridge or to Whitin Community Center to exercise.
Alternatives staff help him get to doctor visits for a hearing aid he wears.
His roommate, Mr. Paquette, said he goes to the doctor for his glasses.
Across the Mumford River from the Whitin Mill, in the former Whitin Machine Works, four people served by Alternatives are working with two staff members on communication skills at the Adult Learning Center, a day habilitation center funded by MassHealth.
One of the men, Dirk Fuller, uses an iPad and points to letters to help him communicate.
Besides being a skill needed to work and interact in society, communication is also a big part of behavioral health, Mr. Seibold explained. Frustration over inability to communicate often underlies outbursts or depression.
“The bottom line is, it’s a care coordination service,” Mr. Seibold said about the CCHP community partnership. “If these providers aren’t talking to each other, they end up in the ER.”
He continued, “One of the jobs of the care coordinator is to know all of the services that are out there and make sure these MassHealth recipients are hooked up with everything they need. This ties it all together.”
More than half the people served by Venture Community Services in Sturbridge, another member of CCHP, have multiple diagnoses and are medically complex, according to Michael Hyland, president and CEO. “They’re very much symbolic of people in MassHealth. Very few of them have one need to be met.”
The community partner model will “allow the clock to get ticking faster” and put the right services in place before someone is discharged from the hospital or has a medical crisis.
He said CCHP has been meeting with health centers and ACOs to work out the logistics of referrals and care management.
Behavioral health community partners will have some financial risk sharing from the beginning of the program. Community partners that provide long-term services and support will phase into risk sharing in the third year.
“We have an opportunity to participate in reshaping the care model in Massachusetts at a pretty high level,” Mr. Hyland said.
“Everybody is going to be in managed care,” said Ms. Jordan of Seven Hills Foundation. “Let’s use our $2 billion (statewide) over the next five years to figure it out together.”

Clinical coordinator Christina Estrada assists Lauren DeMoranville at the “smart board” Feb. 15 at Alternatives in Whitinsville. [PHOTO/EDD COTE]
